Invest to End TB. Save Lives - World Tuberculosis Day 2022
Each year, World Tuberculosis Day is marked on 24th March, the day in 1882 when Dr Robert Koch announced he had discovered the bacterium that causes tuberculosis (TB), opening the way towards diagnosing and curing this disease. To date, TB remains one of the world’s deadliest infectious killers, killing 4100 people every day worldwide. Global efforts to combat TB have saved an estimated 66 million lives since 2000, however, the COVID-19 pandemic has reversed years of progress made in the fight to end TB. (source: the World Health Organization)
The theme for this year’s World TB Day is ‘Invest to End TB. Save Lives.’ and conveys the urgent need to invest more resources to boost the fight against TB and achieve the commitment of ending TB. Equitable access to prevention and care is needed, together with better preventative measures and treatment options.
TB is one of the main BactiVax target infections, our researchers focusing on finding new and improved vaccines against TB, that can prevent or more effectively cure TB. To mark World TB Day, we highlight our researchers’ efforts to end TB.
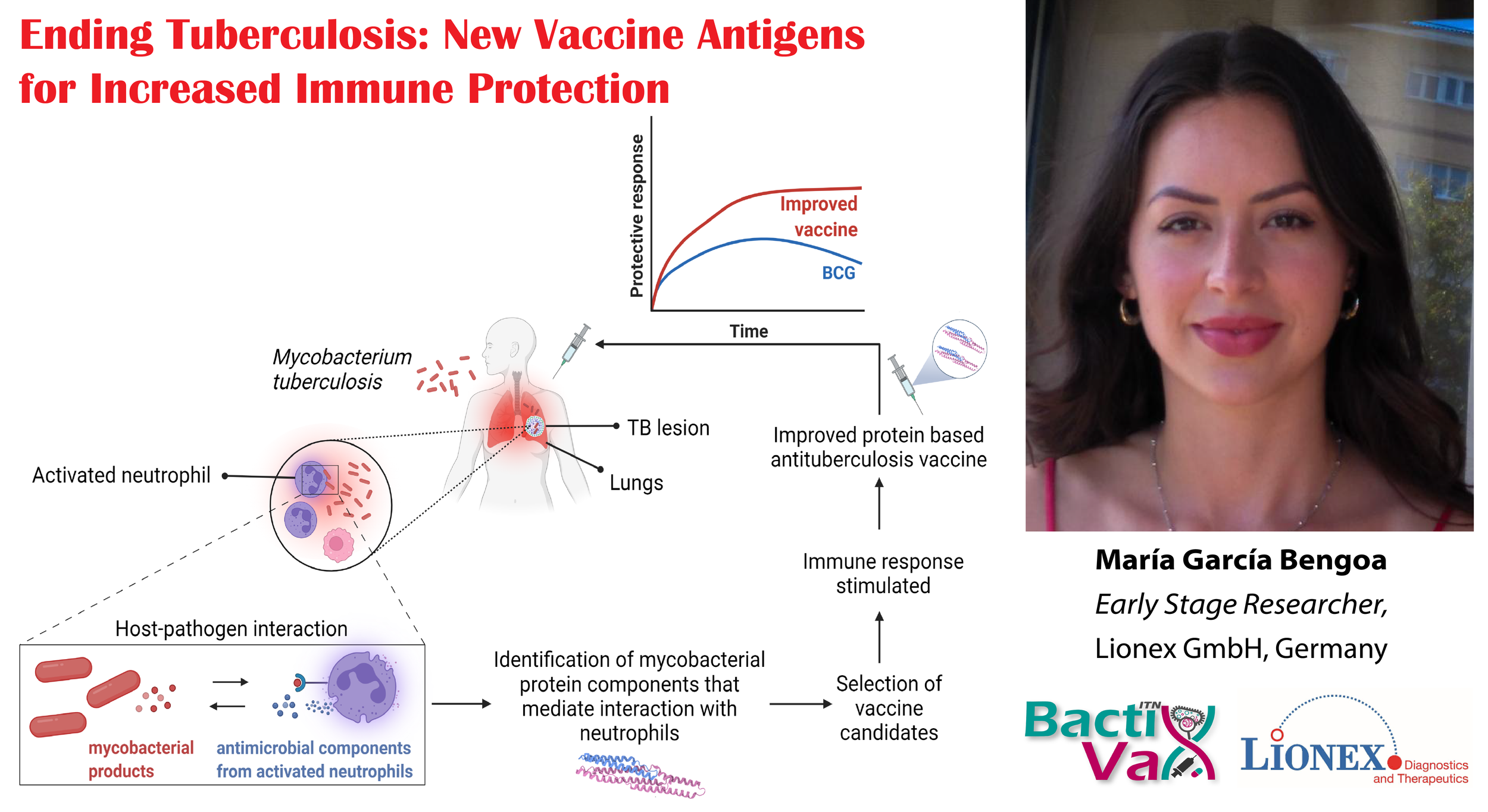
First up we have María García Bengoa, researcher with LIONEX Diagnostics and Therapeutics (Germany), who looks closely at the interaction between Mycobacterium tuberculosis, the pathogen causing TB and our immune cells. Based on this, she selects those bacterial proteins that elicit a specific and optimal immune response, and brings them forward as vaccine antigens.
‘Every year, tuberculosis, TB for short, kills 1.5 million people and causes disease in 10 million people worldwide. TB is a serious infectious disease caused by Mycobacterium tuberculosis (Mtb), a pathogen that enters the respiratory tract through inhalation and affects the lungs. Treatment for TB is long, toxic and expensive, and the existing BCG (Bacillus Calmette-Guérin) vaccine is not completely effective. Thus, new and more effective treatments and vaccines are needed. For this, I aim to identify improved protein vaccine candidates from Mtb by first understanding their interaction with the host through one key immune cell type that first arrives at the site of infection: neutrophils, and secondly, by testing their potential as stimulators of the human immune response.’ - María García Bengoa
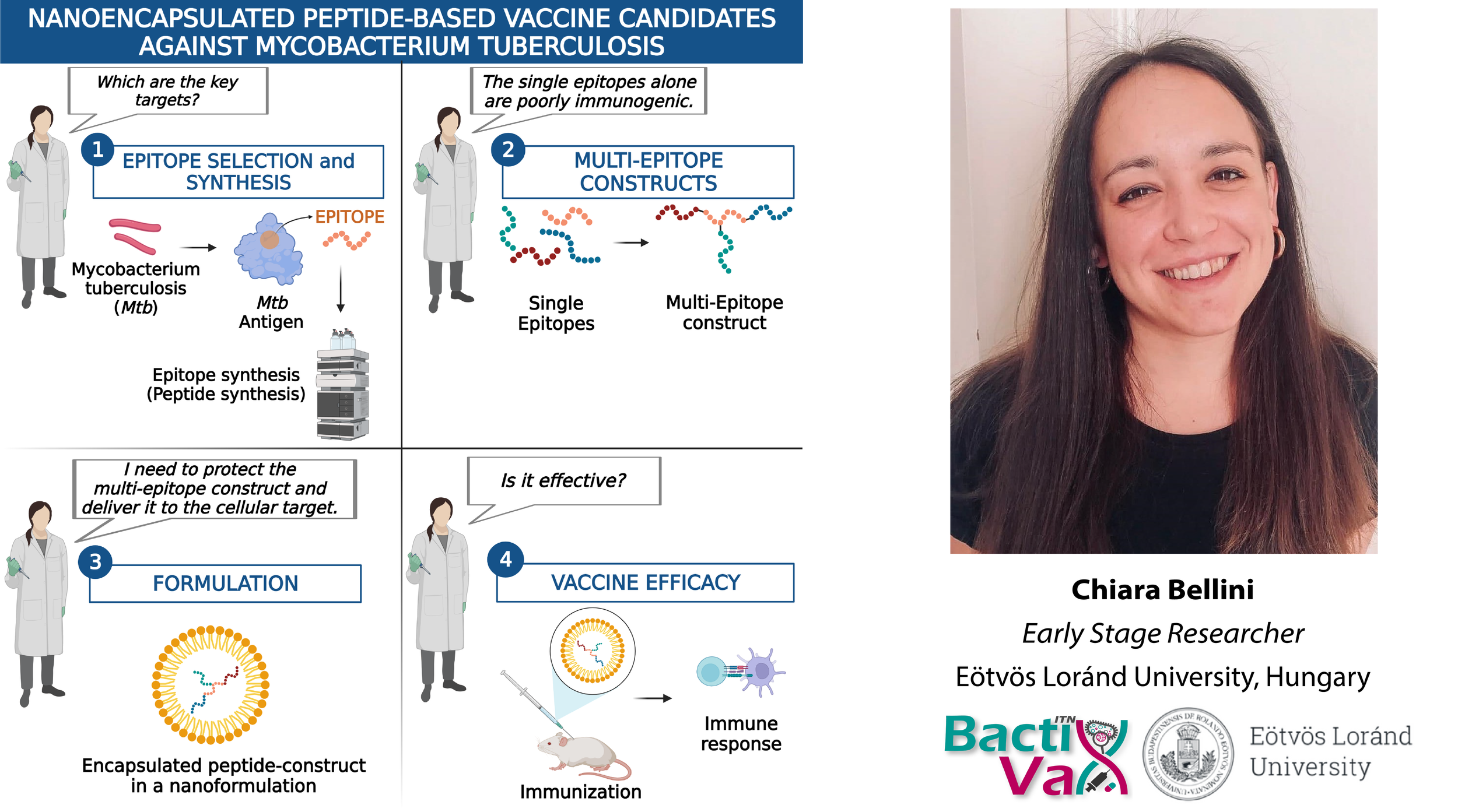
Next we have Chiara Bellini, researcher with Eötvös Loránd University (Hungary), who works on tackling the issue of antigen variability in Mycobacterium tuberculosis (the pathogen causing TB). This is when bacteria change and adapt, causing the immunity elicited by a vaccine or a bacterial strain to fail in protecting against another strain. Chiara's approach in addressing this issue is to develop a synthetic peptide-based vaccine, formulated in a nanocapsule, that can elicit a broad response against #TB and target the immune system more efficiently.
‘The antigen variability is one of the main persistence mechanisms in tuberculosis that makes vaccine development challenging. In my project, I use synthetic peptide-based technology combined with nanotechnology to address the bacteria variability and deliver the “message” to the immune system. In this way, I aim to design a promising vaccine candidate that can promote a broader-action response and protection against the Mycobacterium tuberculosis infection.’ - Chiara Bellini
Emil Joseph Vergara, researcher at St George's, University of London (UK), focuses on the highly problematic multi-drug resistant tuberculosis (MDR-TB). Current treatment options for MDR-TB include a cocktail of at least 4 antibiotics, that needs to be taken for up to 18 months and has a cure rate of only 55%. Through a combination of post-exposure vaccination or immunotherapy with antibiotics, Emil aims to significantly improve MDR-TB outcomes by increasing treatment effectiveness, while reducing duration and toxicity.
‘Treatment of multi-drug resistant Tuberculosis (MDR-TB) using a cocktail of at least four antibiotics typically lasts for up to 18 months. Aside from the toxic effects of long-term antibiotic treatment, the financial burden of MDR-TB infection comes at a huge personal cost for those who suffer from the disease. More importantly, the cure rate for MDR-TB is low, with only 55% getting successfully cured. The aim of my project is to provide proof-of-concept that the administration of a post-exposure vaccine or combined immunotherapy can improve treatment outcomes when used alongside conventional antibiotic therapy.’ - Emil Vergara
Recent tweets from BactiVax
-
RT @mcclean_siobhan: Our fantastic @Bactivax meeting is all over. Great science, great chats and plenty of fun. Thanks to Rita Berisio (… https://t.co/sC7ddNvinE
-
RT @mcclean_siobhan: We had a really informative session this morning on D3 of our @BactiVax summer school: Science Communication & over… https://t.co/sj3zYNHs0h
-
RT @mcclean_siobhan: Amazing talk from Mariagrazia Pizza from @GSK who shared her extensive experience in working on Bacterial #Vaccines… https://t.co/Nm4U46hxJd
-
RT @mcclean_siobhan: Amazing day and it’s been wonderful to see the research projects of each #ESRs develop and grow. 🎉🎉🎉 @REA_research
-
RT @mcclean_siobhan: @LorenzoBossi5 was our last speaker of the day. Based at @immunxperts, he presented his work on the human immune re… https://t.co/THA1OkaxT3
Check us out on Instagram too